- Research
- Open access
- Published:
Association of the TRIM family protein with survival outcomes and clinicopathological features in colorectal cancer: a systematic review and meta-analysis
BMC Cancer volume 24, Article number: 537 (2024)
Abstract
Background
The tripartite motif (TRIM) proteins have been reported to play crucial roles in various malignancies. However, the clinical significance of TRIM proteins in colorectal cancer (CRC) remains controversial. This study aimed to evaluate the association between TRIM proteins and the clinicopathological features and survival outcomes in patients with CRC.
Methods
We performed a meta-analysis to investigate whether TRIM is a prognostic factor in CRC. PubMed, Embase, Web of Science, CNKI and Weipu databases were searched to identify eligible studies that evaluated the association between TRIM proteins and overall survival (OS), as well as the clinicopathological features of patients with CRC. Hazard ratios (HR) or odds ratios (OR) with 95% confidence interval (CI) were derived and pooled using a fixed-effects model.
Results
From inception to March 2023, we extracted study characteristics and prognostic data for each identified study. Twelve studies enrolling 1608 patients were eligible for inclusion. Data on OS and recurrence-free survival (RFS) were available for 12 and 2 studies, respectively. The pooled analysis results showed a significant correlation between the elevated TRIM proteins and shorter OS (HR = 2.42, 95% CI: 1.96–2.99) and worse RFS (HR = 2.51, 95% CI: 1.78–3.54) in patients with CRC. The combined ORs indicated that TRIM protein over-expression was significantly associated with advanced TNM stage (OR = 2.26, 95% CI: 1.25–4.10), deep tumor invasion (OR = 2.01, 95% CI: 1.04–3.88), lymph node metastasis (OR = 2.99, 95% CI: 2.19–4.09) and perineural invasion (OR = 1.95, 95% CI: 1.18–3.23).
Conclusions
Our findings suggest that TRIM proteins can predict tumor progression and poor prognosis in CRC. Therefore, TRIM proteins may be promising therapeutic targets for patients with CRC.
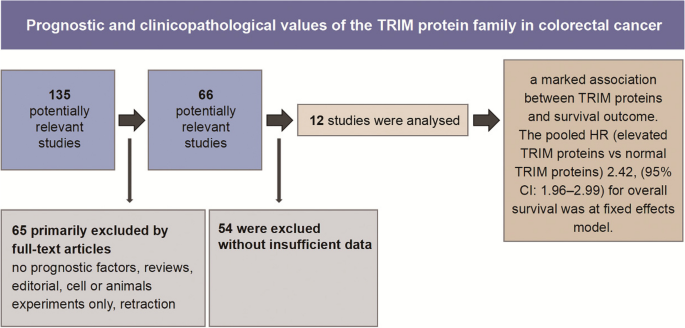
Graphical Abstract
Introduction
Colorectal cancer (CRC) is a common malignant cancer in both males and females and is the second leading cause of cancer-related deaths worldwide [1]. Despite a slight decrease in mortality due to enhanced detection techniques and ever-improving therapeutic approaches, patients with CRC still exhibit poor survival owing to the rising metastatic capacity of primary tumors and high recurrence rate [2, 3]. Recently, numerous studies have concentrated on novel biomarkers for the clinicopathological characteristics and prognosis of patients with CRC, with the aim of identifying new therapeutic targets [4, 5].
The tripartite motif (TRIM) family of proteins is characterized by an N-terminal TRIM containing a RING-finger domain, one or two zinc-finger domains known as a B-box and a coiled-coil region [6]. Owing to the RING-finger domain, TRIM proteins possess E3 ligase activity and participate in the degradation of a series of proteins. TRIM proteins have been reported to play crucial roles in various biological behaviors, and their dysregulation contributes to oncogenesis and tumor progression [7, 8]. Several studies have examined the prognostic role of different TRIM proteins in various malignancies [9,10,11]. However, the prognostic role of the TRIM protein family in CRC remains unclear.
Therefore, we conducted a systematic review and meta-analysis to evaluate the association between TRIM proteins and the clinical outcomes in patients with CRC. Understanding TRIM proteins can considerably contribute to their validations as promising novel biomarkers and potential therapeutic targets for CRC.
Materials and methods
The present study was conducted according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses [12]. We registered on PROSPERO (CRD42023417799) before conducting the literature search.
Search strategy
Two independent researchers systematically searched the Web of Science, PubMed, Embase, CNKI and Weipu electronic databases from their inception to March 1, 2023. No language restrictions were imposed. The following medical subject headings or keywords were adopted according to the retrieval strategy: ‘trim’ OR ‘trim family’ OR ‘trim proteins’ OR ‘tripartite motif’ OR ‘tripartite motif proteins’; ‘cancer’ OR ‘tumor’ OR ‘carcinoma’ OR ‘neoplasm’; ‘colon’ OR ‘rectum’ OR ‘colorectal’. To avoid ignoring qualified studies, all references of the selected primary studies were screened.
Inclusion and exclusion criteria
First, based on the pre-specified selection criteria, two independent researchers screened titles and abstracts to exclude irrelevant studies. Duplicate studies were also excluded from analysis. Next, the full text of all potentially pertinent studies were assessed according to the following inclusion criteria: (1) the expression of TRIM proteins was detected in primary tumor tissues after surgical resection; (2) all patients included were divided into two or more groups based on the TRIM expression levels; (3) the hazard ratio (HR) of survival outcomes or clinicopathological features related to high and low levels of TRIM expressions were available; and (4) the survival curves or sufficient data were available to calculate the HR with 95% confidence interval (CI).
The exclusion criteria were as follows: (1) studies without prognostic outcomes; (2) studies with insufficient data for analysis; and (3) study designs of reviews, case reports, conference abstracts, editorials and letters.
Data extraction
The following data were independently collected by two investigators from eligible studies: first author, year of publication, country, sample capacity, duration of follow-up, overexpression rate, detection method and outcome measures. The data were extracted into a predefined table. Additionally, information was collected on the clinicopathological parameters related to tumor progression. For survival outcome extraction, the HRs and 95% CIs were directly collected from the multivariate and univariate analysis calculated by Cox proportional hazards regression model. We extracted the crude HR and 95% CIs from the univariate analysis and the adjusted HR and 95% CIs after adjustment for potential confounders from the multivariate analysis. Engauge Digitizer version 4.0. was used to estimate survival statistics if Kaplan–Meier curves were only provided. Disagreements between the two reviewers were verified after a discussion and review of the trial information.
Quality assessment
The quality of the enrolled studies was assessed using the Newcastle–Ottawa quality assessment scale, which consists of three main aspects: (1) selection of the research groups, (2) comparability of the groups and (3) ascertainment of the exposure or outcome [13].
Statistical analysis
The relationship between the expression of TRIM proteins and prognosis, as well as the clinicopathological features of CRCs, was analyzed using STATA/SE 17. To estimate the potential heterogeneity among the included studies, I2 statistics and the Chi-square Q test were employed. A fixed-effects model was applied to pool the HR of each eligible study into a summary HR if there was no obvious heterogeneity (I2 < 50% or PQ ≥ 0.10). In contrast, when heterogeneity was considered significant (I2 ≥ 50% or PQ < 0.10), the random-effects model was adopted. The sources of heterogeneity were explored using subgroup or meta-regression analyses to examine all possible factors. Funnel plots and Egger’s and Begg’s tests were performed to assess the risk of publication bias [14]. Sensitivity analysis was performed to ensure the stability of the summarized results. In the present study, *P < 0.05 indicated a significant difference.
Results
Characteristics of eligible studies
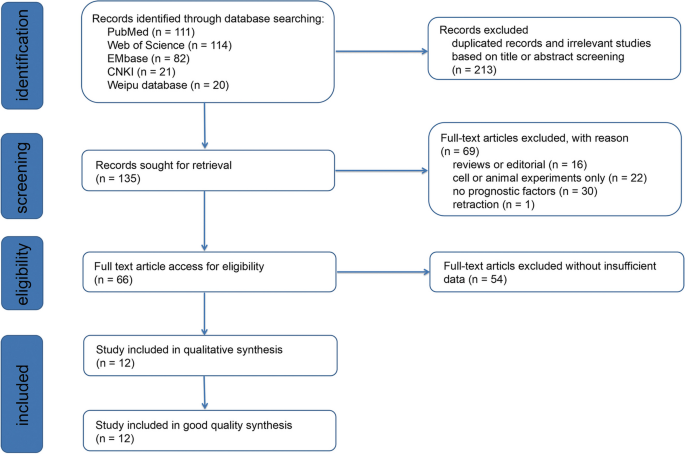
Details of the meta-analysis search process are shown in Fig. 1. Using a database search, 135 articles were initially identified, after removing duplicates. Following the removal of reviews and articles focusing on cellular or animal experiments, 66 studies remained for further reading. Finally, 12 articles with 1608 patients in total were included in the present meta-analysis based on the bias of the inclusion and exclusion criteria abovementioned [15,16,17,18,19,20,21,22,23,24,25,26]. The lack of sufficient data for analysis was the most common reason for exclusion during the full-text review process.
The characteristics of the included 12 studies are summarized in Table 1. Among the 12 eligible studies published from 2013 to 2020, one was from Ireland and the remaining 11 were conducted in China. Seven of 12 studies didn’t report the follow-up duration. Two study’s follow-up time were at least 40 months and 60 months respectively. The median follow-up duration is 54 months (range 1–122 months) in Seán Fitzgerald’s research, 60 months in Zhang Y’s study and 43.6± 38.4 months (range, 4–132 months) in Li CG’s work. Twelve studies reported the overall survival (OS) of patients with CRC, whereas two studies reported an association between recurrence-free survival (RFS) and TRIM proteins. The expression of TRIM proteins in tissue samples and adjacent non-tumor tissues was detected by immunohistochemistry. Most of the enrolled studies performed univariate and multivariate Cox regression analyses; otherwise, Kaplan–Meier Curves were provided. The crude and adjusted HR values reported by univariate and multivariate analysis and HR extracted by Kaplan-Meier curves are listed in Supplementary Table 1.
All enrolled articles, ranging from six to nine, were assessed to be of high quality based on the Newcastle–Ottawa quality assessment scale.
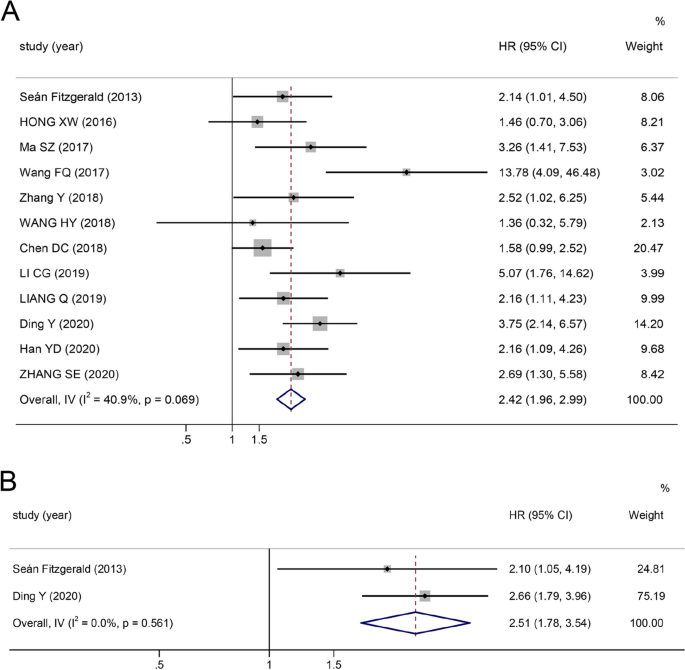
Correlation between increased TRIM expression and OS
As is shown in Fig. 2, the summary HR for the OS comparing TRIM proteins over-expression versus low-expression is 2.42 (95% CI: 1.96–2.99, ***P ≤ 0.0001), and moderate heterogeneity between studies (I2 = 40.9%, P = 0.069) is observed. Elevated TRIM expressions in CRC tissues are strongly associated with poor OS, indicating that elevated TRIM protein levels could serve as a poor prognostic indicator in CRC. In addition, considering the presence of heterogeneity, subgroup analyses were performed according to the following three parameters: cut-off value (final staining scores, percentage of positive cells and others), sample size of studies (≥ 100 and < 100) and analysis type (multivariate and survival curves). Pooled analysis results demonstrated that all subgroups were in accordance with the OS as abovementioned (Supplementary Table 2); however, a possible interaction was noted between the analysis type and sample size subgroups. The heterogeneity was clearly decreased in the analysis type (I2 = 0.0%) and sample size (I2 = 27.1%) subgroups, suggesting that different types of analyses and sample capacity may result in the main heterogeneity among the correlations between the overexpression and OS.
Correlation between increased TRIM expression and RFS
As shown in Fig. 2, the pooled HR demonstrates that a high level of TRIM expression is associated with poor RFS (HR 2.51, 95% CI: 1.78–3.54, ***P ≤ 0.0001). No heterogeneity was observed among the studies (I2 = 0.0%, P = 0.561).
Correlation between increased TRIM expression and clinicopathological features
To assess the risk of TRIM overexpression under different clinicopathological features, the pooled odds ratios (ORs) were calculated (Table 2). The results revealed that a high-level expression of TRIM was associated with an advanced TNM stage (OR = 2.26, 95% CI: 1.25–4.10), deeper depth of tumor invasion (OR = 2.01, 95% CI: 1.04–3.88), poor tumor differentiation (OR = 0.63, 95% CI: 0.44–0.90), lymph node metastasis (OR = 2.99, 95% CI: 2.19–4.09) and perineural invasion (OR = 1.95, 95% CI: 1.18–3.23). Conversely, no significant association was observed between up-regulated TRIM expressions and gender (OR = 1.04, 95% CI: 0.82–1.33, P = 0.725), tumor location (OR = 0.93, 95% CI: 0.65–1.33, P = 0.673) or distant metastasis (OR = 0.92, 95% CI: 0.39–2.19, P = 0.855).
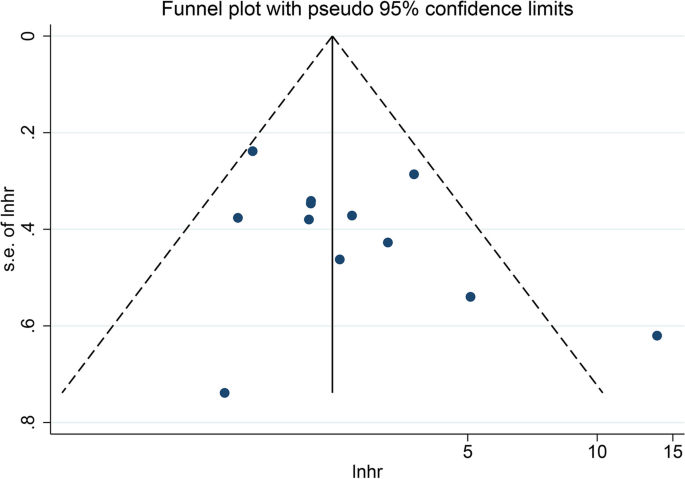
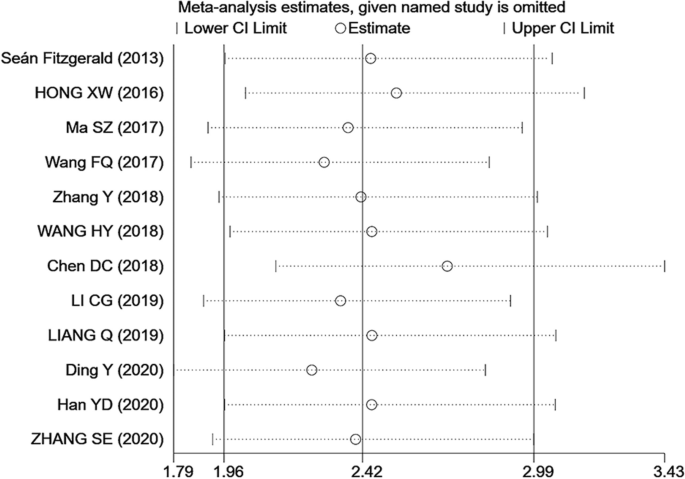
Publication bias and sensitivity analysis
Funnel plot and Begg’s and Egger’s tests were used to test for publication bias. The funnel plot for OS did not show any obvious publication bias (Fig. 3). The results of Begg’s (P = 0.244) and Egger’s (P = 0.184) tests were not significantly different (Supplementary Figure S1); therefore, no significant publication bias occurred in the present meta-analysis. In addition, sensitivity analysis (Fig. 4) showed that even after sequentially omitting the included articles, the pooled results of the meta-analysis were still relatively robust.
Discussion
Thus far, more than 80 TRIM proteins have been discovered and shown to be involved in the tumor progression of various malignancies [27]. Numerous TRIM proteins are implicated in the ubiquitination–proteasome system as E3-ubiquitin ligases. Therefore, they regulate diverse cellular processes, including proliferation, differentiation, signal transduction, autophagy and protein stability, which can result in tumorigenesis in an increasingly specific and important manner [8]. Numerous TRIM family members have been reported to be overexpressed in one or more cancers, such as hepatocellular carcinoma, gastric, lung and pancreatic cancers and breast carcinoma [28,29,30]. In contrast to non-tumor tissues, CRC tissues show higher levels of TRIM52 expression, and elevated TRIM52 levels are significantly correlated with the proliferation, migration and invasion of CRC cells [31]. TRIM59 is also upregulated and associated with tumor size and lymph node metastasis, indicating poor prognosis in CRC [32]. The upregulation of distinct TRIM family members is correlated with poor overall survival outcomes among cancer patients; therefore, TRIM proteins have excellent potential as biomarkers for cancer prognosis.
Recent studies have aggregated the functions of certain TRIM family members in cancer prognosis according to diverse tumor types. For instance, Hu et al. estimated the mortality risk in a relatively large population composed of 7239 participants in 17 studies, which showed that high expression of TRIM21 was significantly correlated with improved OS and progression-free survival in various cancers [33]. A meta-analysis by Xiao et al. reported that overexpression of TRIM44 was significantly correlated with not only shorter over-survival and worse disease-free survival, but also tumor metastasis, poor tumor differentiation, deeper tumor invasion and advanced clinical stage [34]. Both Xue et al. and Yuan et al. reported that upregulated TRIM24 expression significantly predicts poor overall survival in different types of malignancies [35, 36]. Whether the overexpression of TRIM proteins could be useful in predicting the prognosis of patients with CRC remains unclear.
To our knowledge, our meta-analysis is the first systematic review and meta-analysis to assess the prognostic and clinicopathological values of TRIM proteins for patients with CRC. Herein, the pooled results of 1608 participants with CRC from 12 eligible studies indicated that patients with CRC with elevated TRIM protein expressions had significantly shorter OS and worse RFS than those with normal TRIM expressions. In the meta-analysis of OS, moderate heterogeneity was observed (I2=40.9%, P = 0.069). However, subsequent subgroup analyses further confirmed that the cut-off value, sample size and type of analysis did not significantly affect the results. Moreover, sensitivity analyses were performed by omitting one study at a time, and publication bias tests did not significantly influence the results. Therefore, the overexpression of TRIM proteins may be positively correlated with poor prognosis. TRIM28, which is highly expressed in patients with CRC, is an independent prognostic marker for OS, with a pooled HR of 2.57 in two different prospective studies by Fitzgerald et al. and Ma et al., with a total of 202 patients with CRC (Supplementary Figure S2) [15, 17].
Because the clinicopathological features in different groups of patients affect their outcomes, eight major factors between patients with upregulated and normal TRIM expressions were compared. The overexpression of TRIM proteins was markedly associated with higher TNM stage, deeper invasion, lymph node metastasis and perineural invasion. Notably, patients with higher levels of TRIM proteins exhibited an enhanced degree of tumor histological differentiation, which contradicts previous studies [34]. Thus, more studies with larger populations should be conducted in the future to confirm these conflicting results. However, TRIM protein expression was not significantly associated with gender, tumor site or distant metastasis. In the present study, overexpression of TRIM proteins was associated with CRC progression and poor clinical outcomes. An increasing number of studies have demonstrated that TRIM proteins contribute to the diverse malignant biological behaviors of CRC cells. Hence, TRIM proteins have excellent potential to serve as biomarkers for CRC prognosis, and further research should be conducted to investigate the molecular mechanisms and to verify the clinical application of TRIM proteins.
Our systematic review has some limitations. First, most of the studies we chose were conducted in the Chinese population, to the extent that the statistical analysis of publication bias lacked sufficient power. Notably, one study with a high HR was responsible for almost all the observed heterogeneity. However, sensitivity analyses showed that removing this article did not significantly influence the pooled results. Therefore, additional samples from other countries or races should be included to confirm the reliability of these results. Second, we were unable to contact the authors of certain studies to retrieve data. In some articles, HRs and 95% CI were extracted from additional data, such as Kaplan–Meier curves, which might have resulted in an uncertain bias for the pooled estimates. And unfortunately, some studies lack of detailed information, which might result in a lack of control for potential confounding factors. Third, owing to the limited number of studies, heterogeneity still existed in some results of clinicopathological characteristics.
Conclusion
In summary, our current study demonstrates that TRIM proteins are correlated with cancer progression and prognosis in patients with CRC. The TRIM family may be a reliable biomarker for determining the clinicopathological characteristics and prognosis of malignancies. With further understanding of the regulatory mechanisms, TRIM proteins are promising new therapeutic targets for CRC.
Availability of data and materials
All data generated or analysed during this study are included in this published article and its Supplementary information files.
References
Sung H, Ferlay J, Siegel RL, Laversanne M, Soerjomataram I, Jemal A, et al. Global Cancer Statistics 2020: GLOBOCAN Estimates of Incidence and Mortality Worldwide for 36 Cancers in 185 Countries. CA Cancer J Clin. 2021;71(3):209–49.
Siegel RL, Wagle NS, Cercek A, Smith RA, Jemal A. Colorectal cancer statistics, 2023. CA Cancer J Clin. 2023;73(3):233–54.
Brenner H, Kloor M, Pox CP. Colorectal cancer. Lancet Lond Engl. 2014;383(9927):1490–502.
De Sousa E, Melo F, Colak S, Buikhuisen J, Koster J, Cameron K, de Jong JH, et al. Methylation of cancer-stem-cell-associated Wnt target genes predicts poor prognosis in colorectal cancer patients. Cell Stem Cell. 2011;9(5):476–85.
Giovannetti E, Backus HHJ, Wouters D, Ferreira CG, van Houten VMM, Brakenhoff RH, et al. Changes in the status of p53 affect drug sensitivity to thymidylate synthase (TS) inhibitors by altering TS levels. Br J Cancer. 2007;96(5):769–75.
Vunjak M, Versteeg GA. TRIM proteins. Curr Biol CB. 2019;29(2):R42-4.
Hatakeyama S. TRIM Family Proteins: Roles in Autophagy, Immunity, and Carcinogenesis. Trends Biochem Sci. 2017;42(4):297–311.
Mohammadi A, Pour Abbasi MS, Khorrami S, Khodamoradi S, Mohammadi Goldar Z, Ebrahimzadeh F. The TRIM proteins in cancer: from expression to emerging regulatory mechanisms. Clin Transl Oncol. 2022;24(3):460–70.
Marzano F, Caratozzolo MF, Pesole G, Sbisà E, Tullo A. TRIM Proteins in Colorectal Cancer: TRIM8 as a Promising Therapeutic Target in Chemo Resistance. Biomedicines. 2021;9(3):241.
Lu K, Pan Y, Huang Z, Liang H, Ding ZY, Zhang B. TRIM proteins in hepatocellular carcinoma. J Biomed Sci. 2022;29(1):69.
Zhan W, Zhang S. TRIM proteins in lung cancer: Mechanisms, biomarkers and therapeutic targets. Life Sci. 2021;1(268): 118985.
Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;29(372): n71.
Wells G, Shea B, O'Connell J. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomized studies in meta-analyses. Ottawa Health Research Institute Web site. 2014;7(1).
Egger M, Davey Smith G, Schneider M, Minder C. Bias in meta-analysis detected by a simple, graphical test. BMJ. 1997;315(7109):629–34.
Fitzgerald S, Sheehan KM, O’Grady A, Kenny D, O’Kennedy R, Kay EW, et al. Relationship between epithelial and stromal TRIM28 expression predicts survival in colorectal cancer patients: TRIM28 predicts survival in colorectal cancer. J Gastroenterol Hepatol. 2013;28(6):967–74.
Xu W, Xu B, Yao Y, Yu X, Cao H, Zhang J, et al. RNA interference against TRIM29 inhibits migration and invasion of colorectal cancer cells. Oncol Rep. 2016;36(3):1411–8.
Ma SZ, et al. Expression of TRIM28 in colorectal cancer tissues and its effect on the proliferation and migration of cancer cells. Shandong Medical Journal. 2017;57:28–30.
Fengqin Wang. Prognostic relevance of tripartite motif containing 24 expression in colorectal cancer. Pathol - Res Pract. 2017;213(10):1271–5.
Haiyu Wang Lu, Yao Yuda Gong, Zhang Bo. TRIM31 regulates chronic inflammation via NF-κB signal pathway to promote invasion and metastasis in colorectal cancer. Am J Transl Res. 2018;10(4):1247.
Zhang Y, Feng Y, Ji D, Wang Q, Qian W, Wang S, et al. TRIM27 functions as an oncogene by activating epithelial-mesenchymal transition and p-AKT in colorectal cancer. Int J Oncol. 2018;53(2):620–32.
Chen Daici, Li Yichen, Zhang Xiaowen, Haiyong Wu, Wang Qian, Cai Jian, et al. Ubiquitin ligase TRIM65 promotes colorectal cancer metastasis by targeting ARHGAP35 for protein degradation. Oncogene. 2019;38(37):6429–44.
Li CG, Hu H, Yang XJ, Huang CQ, Yu XQ. TRIM44 Promotes Colorectal Cancer Proliferation, Migration, and Invasion Through the Akt/mTOR Signaling Pathway. OncoTargets Ther. 2019;12:10693–701.
Liang Q, Tang C, Tang M, Zhang Q, Gao Y, Ge Z. TRIM47 is up-regulated in colorectal cancer, promoting ubiquitination and degradation of SMAD4. J Exp Clin Cancer Res CR. 2019;12(38):159.
Ding Y, et al. expression of TRIM14 in Colorectal Cancer and Its Clinical Significance. Acta Med Univ Sci Technol Huazhong. 2020;49(3):323–7.
Zheng Shuier, Zhou Chenliang, Wang Yonggang, Li Hongtao, Sun Yong, Shen Zan. TRIM6 promotes colorectal cancer cells proliferation and response to thiostrepton by TIS21/FoxM1. J Exp Clin Cancer Res CR. 2020;28(39):23.
Han Y, Tan Y, Zhao Y, Zhang Y, He X, Yu L, et al. TRIM23 overexpression is a poor prognostic factor and contributes to carcinogenesis in colorectal cancer. J Cell Mol Med. 2020;24(10):5491–500.
Gu J, Chen J, Xiang S, Zhou X, Li J. Intricate confrontation: Research progress and application potential of TRIM family proteins in tumor immune escape. J Adv Res. 2023;S2090–1232(23):00024–3.
Yang X, Zhang Y, Xue Z, Hu Y, Zhou W, Xue Z, et al. TRIM56 promotes malignant progression of glioblastoma by stabilizing cIAP1 protein. J Exp Clin Cancer Res CR. 2022;41(1):336.
Ji J, Ding K, Luo T, Zhang X, Chen A, Zhang D, et al. TRIM22 activates NF-κB signaling in glioblastoma by accelerating the degradation of IκBα. Cell Death Differ. 2021;28(1):367–81.
Liu Y, Tao S, Liao L, Li Y, Li H, Li Z, et al. TRIM25 promotes the cell survival and growth of hepatocellular carcinoma through targeting Keap1-Nrf2 pathway. Nat Commun. 2020;11(1):348.
Guo Y, Zhou Y, Gu X, Xiang J. Tripartite motif 52 (TRIM52) promotes proliferation, migration, and regulation of colon cancer cells associated with the NF-κB signaling pathway. J Gastrointest Oncol. 2022;13(3):1097–111.
Dahpy MA, Salama RHM, Kamal AA, El-Deek HE, Abdel Motaleb AA, Abd-El-Rehim AS, et al. Evaluation of tripartite motif 59 and its diagnostic utility in benign bowel diseases and colorectal cancer. J Biochem Mol Toxicol. 2022;36(7):e23065.
Hu F, Liu Y, Wang F, Fu X, Liu X, Zou Z, et al. Prognostic and clinicopathological significance of TRIM21 in various cancers: A meta and bioinformatic analysis. Medicine (Baltimore). 2023;102(23): e34012.
Xiao G, Yang Q, Bao Z, Mao H, Zhang Y, Lin S. Expression of tripartite motif-containing 44 and its prognostic and clinicopathological value in human malignancies:a meta-analysis. BMC Cancer. 2020;20(1):525.
Xue Y, Ge W, Shi W, Huang W, Wang R. Prognostic role of tripartite motif containing 24 in various human solid malignant neoplasms: An updated meta-analysis and systematic review. Medicine (Baltimore). 2021;100(51): e28383.
He Y, Peng KW, Tang T, Deng L, Ye ZL, Luo MJ, et al. Prognostic Implications of Tripartite Motif Containing 24 Expression Levels in Patients with Solid Tumors: A Systematic Review and Meta-Analysis. Genet Test Mol Biomark. 2019;23(7):473–9.
Acknowledgements
I really appreciate for what Chen Chen, Hua Xian, Chunhua Zhao and Han Min contributed to the study, as well as Editage edited my manuscript.
Funding
This work was supported by the Suzhou Municipal Health Commission (GSWS2021041) and the Postgraduate Research and Innovation Program, Jiangsu Province (KYCX22_1781).
Author information
Authors and Affiliations
Contributions
Ying Wu and Chun-Hua Zhao generated the research question, designed the study and approved the final manuscript. Xian Hua made critical appraisals. Chen Chen, Han Min and Chun-Hua Zhao contributed to critically reviewing and editing of the manuscript with regard to important intellectual content. All authors approved of this final version of the manuscript to be submitted.
Corresponding authors
Ethics declarations
Ethics approval and consent to participate
Not applicable.
Consent for publication
Not applicable.
Competing interests
The authors declare no competing interests.
Additional information
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated in a credit line to the data.
About this article
Cite this article
Wu, Y., Chen, C., Hua, X. et al. Association of the TRIM family protein with survival outcomes and clinicopathological features in colorectal cancer: a systematic review and meta-analysis. BMC Cancer 24, 537 (2024). https://doi.org/10.1186/s12885-024-12280-z
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s12885-024-12280-z